Fetal Echo
Fetal echocardiography is a test similar to an ultrasound. This exam allows your doctor to better see the structure and function of your unborn child’s heart. It’s typically done in the second trimester, between 18 to 20 weeks.

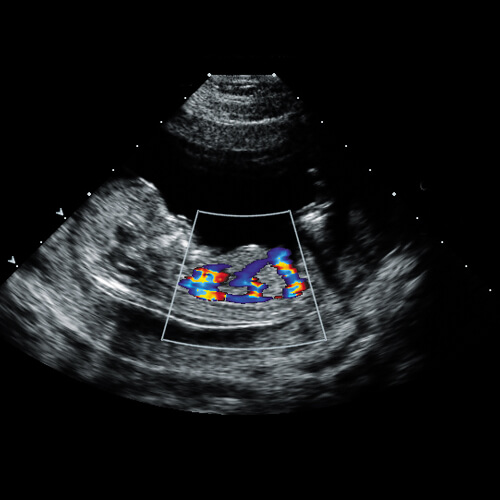
The exam uses sound waves that “echo” off the structures of the fetus’s heart. A machine analyzes these sound waves and creates a picture, or echocardiogram, of their heart’s interior. This image provides information on how your baby’s heart formed and whether it’s working properly.
It also enables your doctor to see the blood flow through the fetus’s heart. This in-depth look allows your doctor to find any abnormalities in the baby’s blood flow or heartbeat.
What is fetal echocardiography ?
Fetal echocardiography is an ultrasound study of the fetal heart before birth to rule out congenital heart disease (CHD).
What is ideal time?
Ideal time for fetal echocardiography is 18-20 weeks, but it can be performed anytime after 16 weeks pregnancy.
Is there any preparation required?
No any special preparation required for fetal echocardiography.
Is this Scan harmful to mother or fetus?
No side effects were noted in the mother or fetus due to fetal echocardiography, as it uses non-audible ultrasound waves not X-ray or radiation.
What are the benefits?
- If normal study it relieves parent stress.
- If cardiac anomaly is detected then parent counselling and help in decision-making can be done for available options for further management according to cardiac anomaly detected – prognostification, time, place & mode of delivery, Early neonatal or perinatal intervention, planned comfort care.
- Parents will be mentally prepared for future management of cardiac anomaly (intervention or surgery).
What is the duration study?
Are all cardiac anomalies can be detected?
Almost all major cardiac anomalies can be detected if fetal echocardiography performed by Expert doctors with appropriate fetal maturity and position, But some minor anomalies like tiny septal defects, bicuspid aortic valve may not be detected by fetal echocardiography. Some cardiac anomalies like PDA & ASD can not be detected or predicted by fetal echocardiography. Some cardiac anomalies are evolving in nature may appear later or after delivery.
Should all pregnant mothers go for fetal echocardiography?
No fetal echocardiography is not mandatory for all pregnant mother, but fetal cardiac screening should be done to all at the time of 18-22 week routine fetal anomaly scan.
Not all pregnant women need a fetal echocardiogram. For most women, a Fetal Anomaly scan will show the development of all four chambers of their baby’s heart.
A Paediatric Cardiologist may recommend that you have this procedure done if previous tests weren’t conclusive or if they detected an abnormal heartbeat in the fetus.
You may also need this test if:
- Your unborn child is at risk for a heart abnormality or other disorder
- You have a family history of heart disease
- You’ve already given birth to a child with a heart condition
- You’ve used drugs or alcohol during your pregnancy
- You’ve been exposed to medications that can cause heart defects, such as epilepsy drugs or prescription acne drugs
- You have other medical conditions, like rubella, type 1 diabetes, lupus, or phenylketonuria
What are the indications for fetal echocardiography?
When is fetal echocardiography used?
1. Previous child had congenital heart disease or family member had heart disease from birth.
2. Suspected cardiac anomaly during routine 18-22 week anomaly scan is the major indication of fetal echocardiography
3. Fetal extra-cardiac anomalies
4. Suspected or diagnosed case of genetic anomaly in fetus
5. Persistent Irregular fetal heart rate (arrhythmias)
6. Thick fetal translucency (NT) in first trimester
7. Fetal hydrops or effusion
8. Monochorionic Twins
9. Maternal diabetes mellitus
10. Maternal phenylketonuria
11. Maternal teratogen exposure – Anti-convulsant drugs, alcohol, retinoic acid, Lithium, NSAIDs, ACE inhibitors, SSRIs
12. Pregnancies by assisted reproductive techniques (ARTs) like IVF (test tube babies),
13. Maternal autoimmune disease SLE, Sjogren syndrome
14. Maternal infection – Rubella, Coxsackie virus, Mumps, Parvo virus
15. Maternal obesity
